"Science": See also carcinogenic gut microbes! Scientists reveal two common bacteria or important drivers of colorectal cancer |
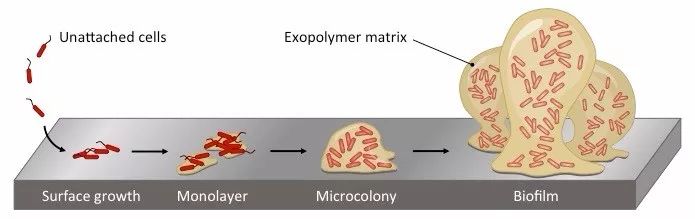
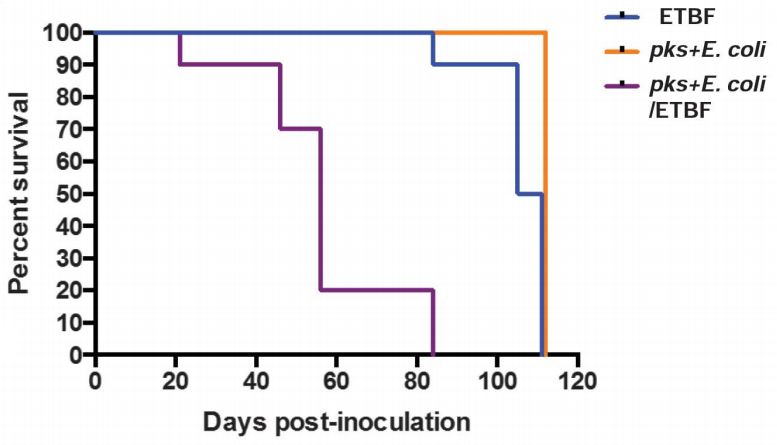
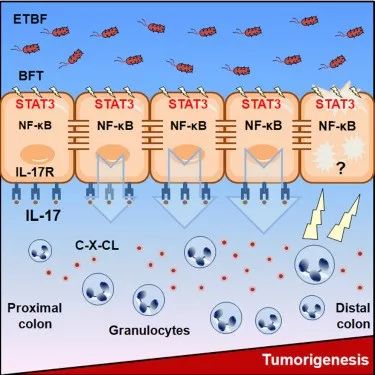
Release date: 2018-02-05 In the past year, the singular cakes introduced a lot of cancer research, from prevention to treatment. Cancer is nothing more than the "gene + environment" interaction. For many cancers, environmental factors are already clear, such as smoking and lung cancer, Helicobacter pylori infection and gastric cancer, as well as high-fat diet and bowel cancer. But there are so few people, they may be "destined" to get bowel cancer when they are born, and it doesn't matter what lifestyle! They are familial adenomatous polyposis (FAP) patients. FAP is caused by mutation of adenomatous polyposis gene (APC), which belongs to autosomal dominant genetic disease. The patient's intestine is covered with large and small polyps, at least 100 or more, up to a thousand, serious The normal intestinal mucosa was hardly observed. If you can't find it early and perform bowel resection, over time, almost 100% of patients will develop colorectal cancer! These hereditary colorectal cancer patients account for about 5% of all colorectal cancer patients [1]. Through previous studies, we know that intestinal microbes play a role in the development of non-hereditary sporadic colorectal cancer (also known as common colorectal cancer), but for hereditary colorectal cancer, microbes also Do you play an important role? Nobody knows~ have said this, and everyone probably guessed it. Yes, new research confirms that the two extremely common gut microbes, E. coli and the special subspecies of Bacteroides fragilis, are the intestines that drive FAP patients. The development of polyposis is a key factor in cancer [2]. Professor Cynthia Sears of the Johns Hopkins Bloomberg-Kimmel Cancer Center led a team to publish a study on Science. They found that the enterotoxin-producing Bacteroides fragilis (ETBF) can "swallow" some of the intestinal mucus and destroy the intestine. The barrier, which itself invades the inner layer of the intestinal mucus with E. coli (pks + E. coli) containing the "genotoxic island" sequence encoded by the polyketide synthase gene (pks), and forms a biofilm [2]. The biofilm is highly resistant to the host's immune system, enveloping the bacteria together, and includes some nutrients that help the bacteria grow and multiply, forming a micro-environment that is “wind and rainâ€. The mucus layer is adjacent to the intestinal epithelial cell layer. The toxins produced by these two bacteria have been shown to induce DNA damage in cells, and chronic inflammation promotes the development of colorectal cancer [3,4]. The researchers examined the intestinal tissue of six FAP patients who underwent resection. They found that 70% of the bacteria in the intestinal mucosa were plaque-like and appeared to be "streaked". Obviously, this small A "plaque" is a biofilm bacterial polymer. Patients with oral antibiotics within 24 hours prior to resection did not find such biofilms. The process of biofilm formation, some individual bacteria → a layer of bacteria → small bacterial community → biofilm Through sequencing, the researchers found that the two most important bacteria in the biofilm are pks+E. coli and ETBF. In the FAP mouse model of APC mutation, they found the same phenomenon as the patient. The researchers compared the intestinal tissue samples of 25 patients with FAP and 23 healthy subjects. The proportion of pks+E. coli and ETBF in FAP patients was significantly higher than that in healthy people (68%, 60%). Vs22%, 30%). The researchers tried to colonize the two bacteria separately or together with sterile mice treated with carcinogenic chemicals. It was found that only a few of the colonized mice developed tumors, regardless of which bacteria were colonized. And the two colonized together have unfortunately suffered from bowel cancer in the same time. This result was also replicated in FAP mice. The mice transplanted with both strains rapidly lost weight. At the 8th week, the tumor died 80%, and the remaining 20% ​​failed to survive the 12th week. . In sharp contrast, the two groups of mice transplanted with ETBF or pks+ E. coli alone still had 90% and 100% survival at week 15. Moreover, mice colonized with both bacteria have higher levels of early inflammation, which is one of the reasons for the development of tumors. That is to say, these two kinds of bacteria are to be hooked together to promote the formation of tumors. It is impossible to fight alone. Survival rate of FAP mice with ETBF (blue), pks+ Escherichia coli (purple) and two colonies (orange) separately over time Although the level of early inflammation is higher, histopathological evaluations show that the overall inflammatory level difference within 15 weeks is not particularly pronounced for single- and post-colonized mice, and overall inflammatory levels do not explain tumor formation. Great difference on the. So where is the problem? Researchers believe that it should be a certain type of inflammation that provokes the girders. This thought reminded Professor Sears of his own research published in the journal Nature Medicine in 2009. She found that interleukin-17, an inflammatory factor, is the key to ETBF-induced tumor formation [4], so this time she will pay attention again. The point is concentrated on the interleukin 17. Further experiments have found that mice that are unable to produce interleukin 17 due to genetic defects do not develop tumors even if they are colonized together. Therefore, inflammation caused by interleukin-17 is the key. The day before the study was published, Professor Sears published a study on the mechanism of ETBF-induced colorectal cancer in Cell Host & Microbe, which is a supplement to this new study. She found that the toxin produced by ETBF (BFT) triggers the production of interleukin-17 by colonic immune cells. This inflammatory molecule acts directly on colonic epithelial cells, further activating the NF-κB pathway and Stat3 protein that promote inflammation, which induces some signaling molecules upon activation. The release of (CXC chemokine) recruits more immune cells to participate in the inflammatory response and promote tumorigenesis [5]. In previous studies, the team found that biofilms were detected early in the carcinogenesis of patients with sporadic colorectal cancer, and biofilm formation is an important factor in the development of tumors [6,7]. Moreover, although the mutation of the APC gene is a direct cause of FAP, there is also a mutation in APC in patients with sporadic colorectal cancer. Therefore, the significance of this study is not only to understand how FAP patients develop colorectal cancer, but also for sporadic patients with APC mutations. Professor Sears said the two studies provide ideas for new strategies to prevent colorectal cancer, such as using probiotics to stop the colonization of two toxins, or developing targeted drugs or vaccines against the toxins they produce. Containment during the development of cancer [1]. Reference materials: [1] https:// [2] http://science.sciencemag.org/content/359/6375/592 [3] Arthur JC, Perez-Chanona E, Mühlbauer M, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota [J]. science, 2012, 338(6103): 120-123. [4] Wu S, Rhee KJ, Albesiano E, et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses [J]. Nature medicine, 2009, 15(9): 1016. [5] http://(18)30042-8 [6] Dejea CM, Wick EC, Hechenbleikner EM, et al. Microbiota organization is a distinct feature of proximal colorectal cancers [J]. Proceedings of the National Academy of Sciences, 2014, 111(51): 18321-18326. [7] Johnson CH, Dejea CM, Edler D, et al. Metabolism links bacterial biofilms and colon carcinogenesis [J]. Cell metabolism, 2015, 21(6): 891-897. Source: Singularity Network
The wheelchair is ideal for transporting immobile patients in hospitals, practices and care facilities. Some wheelchairs can be folded to provide a space-saving storage solution when it is not being used or when taking it along in a medical transport vehicle. Additionally, wheelchairs used in medical facilities should be as robust as possible so that obese patients can also be safely transported. Steel wheelchair and Aluminum wheelchair are available in Yingmed. Commode wheelchair is special for those who are not convenient to stand up to have urine.
Yingmed also supply other Walking Aids like Stand Walker, Underarm crutch and Walking stick. You will find them in the category of Walikng Aids.
Wheel Chair,Aluminum Shower Chair,Bathroom Chair With Wheels,Aluminum Swivel Shower Chair NINGBO YINGMED MEDICAL INSTRUMENTS CO.,LTD , https://www.chinayingmed.com